Call Us Now :
9807 55 6789
-
Call Us Now: 9807 55 6789Call Us Now: 9807 55 6789
Home » THE SCIENCE BEHIND PAIN: HOW YOUR BODY PROCESSES PAIN SIGNALS

Pain globally is a growing problem. Statistics reveal 20 percent adults worldwide suffer from pain. 10 percent each year are newly diagnosed with chronic pain.
This problem is also prevalent in India. However, details are rather sketchy. A 2022 study report revealed that 19 percent Indian adult population suffered from chronic pain of one kind or the other. Pain was especially more prevalent in females with 25 percent. Experts however term these statistics as just a tip of the iceberg since a majority of people don’t reveal their health issues and concerns.
Pain be it a headache or a throbbing ache of an injury, serves a crucial purpose. It acts as the body’s alarm system giving a signal that something is wrong.
It indicates an unpleasant sensory and emotional experience. An experience that’s associated with potential or actual tissue damage. It can be
Pain is classified into two main categories.
Both involve a complex series of processes. The processes are used by the body to signal distress; and protect itself from further harm.
A highly sophisticated communication system is at work when pain is experienced.
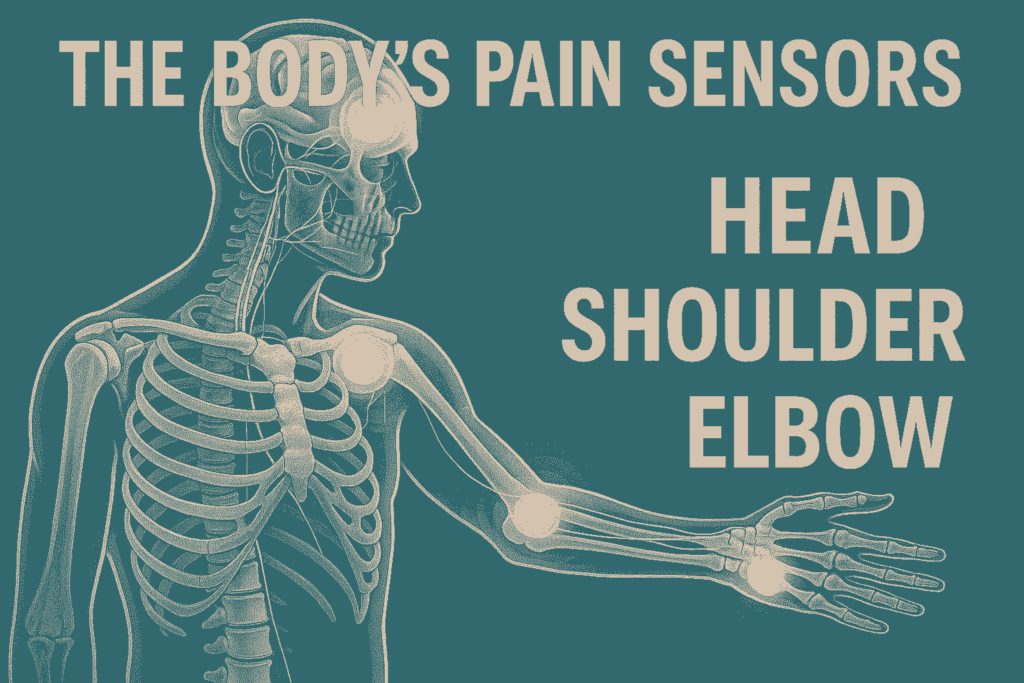
Its signals travel through a series of pathways in the body. Receptors, nerves, and the brain all play pivotal roles.
The following tells about pain transmission process.
The journey of the pain begins at the nociceptors (specialized nerve receptors). They are located throughout the body. That is, from skin to muscles, joints, and internal organs. Noxious stimuli activate them. Stimuli like extreme heat, pressure, or chemicals released during tissue injury.
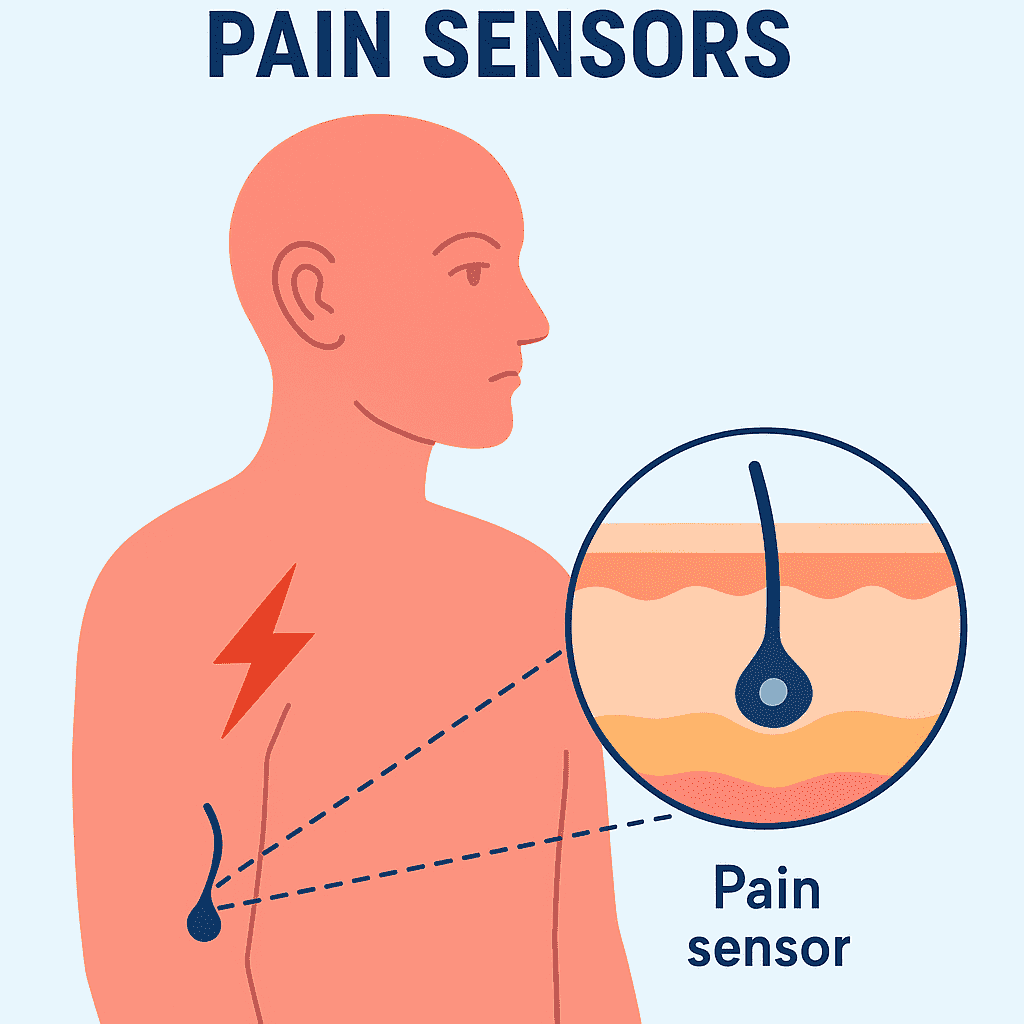
They generate when harmful stimuli are detected by nociceptors electrical signals traveling along nerve fibers toward the spinal cord.
They can be based on the type detected by these receptors be broadly classified into,
The electrical signals once nociceptors are activated gets transmitted via nerve fibers called afferent fibers. These fibers come in two main types,
These signals travel toward the spinal cord along the nerves. There they make their first stop at a crucial relay station called as the Dorsal Horn. This is where the pain signals are processed. Later, are sent on their way to the brain.
The spinal cord acts to the pain signals as a kind of gateway. Additionally, the Dorsal Horn contains complex network of neurons. They decide which pain signals get transmitted to the brain.
Pain when it reaches the spinal cord signals to the brainstem and higher brain centers. Higher bran centers includes the Thalamus, Somatosensory Cortex, and Limbic System.
The Thalamus functions as a relay center. It directs to the appropriate brain areas’ pain signals for processing.
Pain is a physical sensation. It is also an emotional experience. This is why chronic pain affects a person significantly. They can affect mental health, mood, and overall quality of life.
Pain may to irritation or injury seem a straightforward response. However, your body has an array of mechanisms. They can modulate and control how pain is perceived.
This modulation can either amplify or dampen pain signals. This depends on the prevalent circumstances.
It’s among the most important pain-modulating mechanisms.
It was in 1965 that Melzack and Wall proposed this theory.
According to this theory, pain signals’ intensity does not alone determine pain perception. It is also determined by signals processed by the nervous system.
There is a ‘GATE’ in the spinal cord.
This can
Be influenced by varied factors. Including other sensory inputs like touch or pressure. Rubbing a sore area or applying heat to an injury for instance can by activating other sensory nerves which “close the gate” help alleviate pain. This will later reduce the transmission of pain signals.
Pain perception is psychological. It is also influenced by psychological factors. Like attention, mood, past experiences, and expectations. They can all alter how pain is perceived.
People who are anxious or stressed for instance tend to perceive pain intensely. Much more than those who are relaxed. Similarly, focusing on painful stimulus can increase its perceived intensity. Distraction techniques on other hand can reduce the pain’s sensation. Techniques like deep breathing or engaged in enjoyable activity.
Chronic pain is when compared to acute pain a different kind of pain.
Acute pain is a response to illness or injury. Chronic pain on other hand persists for more than three months. It may continue even after the treatment or resolution of the pain’s initial cause. Conditions like Arthritis, Back Pain, and Fibromyalgia, are common examples.
Chronic pain
Better understanding of pain’s mechanism has proved highly beneficial.
They have driven in pain management rapid advancements.
Today, there are varied treatments.
Opioids are commonly used to manage moderate to severe pain. Like Codeine and Morphine. But they can lead to addiction and misuse. As a result, there is greater focus on non-addictive alternatives. Like Acupuncture, CBD (Cannabidiol), and Physical Therapy.
Future pain management could involve
Pain is a complex, multifaceted medical phenomenon. It involves between the body and brain, intricate communication. From the moment you injure yourself, an elaborate system of chemicals, nerves, and brain centers work together till the point where your brain interprets the pain. They create the sensation of pain.
Pain can be unpleasant. However it serves as a protective shield. It helps to prevent further harm to the body. Rapid advances in pain analysis and treatment to better ways to manage pain have significantly helped patients. They can now better cope with the complexities of pain.
We will continue to see the evolution of pain. This provides a ray of hope to people suffering from debilitating chronic or severe pain.
Join our mailing list to get updates about our services and procedures or any events and discounts.

Indo-British Advanced Pain Clinic © 2026. All Rights Reserved. Designed & Developed By Adroit
WhatsApp us